Navigating irritable bowel syndrome can feel daunting, but recognizing IBS symptoms is a critical first step towards effective management.
Understanding Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome is a perplexing condition that affects the delicate balance of our digestive system. Unlike more severe gastrointestinal disorders, IBS doesn’t cause permanent damage or increase the risk of colon cancer. However, its unpredictable nature and array of symptoms can significantly impact one’s quality of life. To better understand this condition, let’s dive into the key characteristics that define IBS.
Defining Irritable Bowel Syndrome
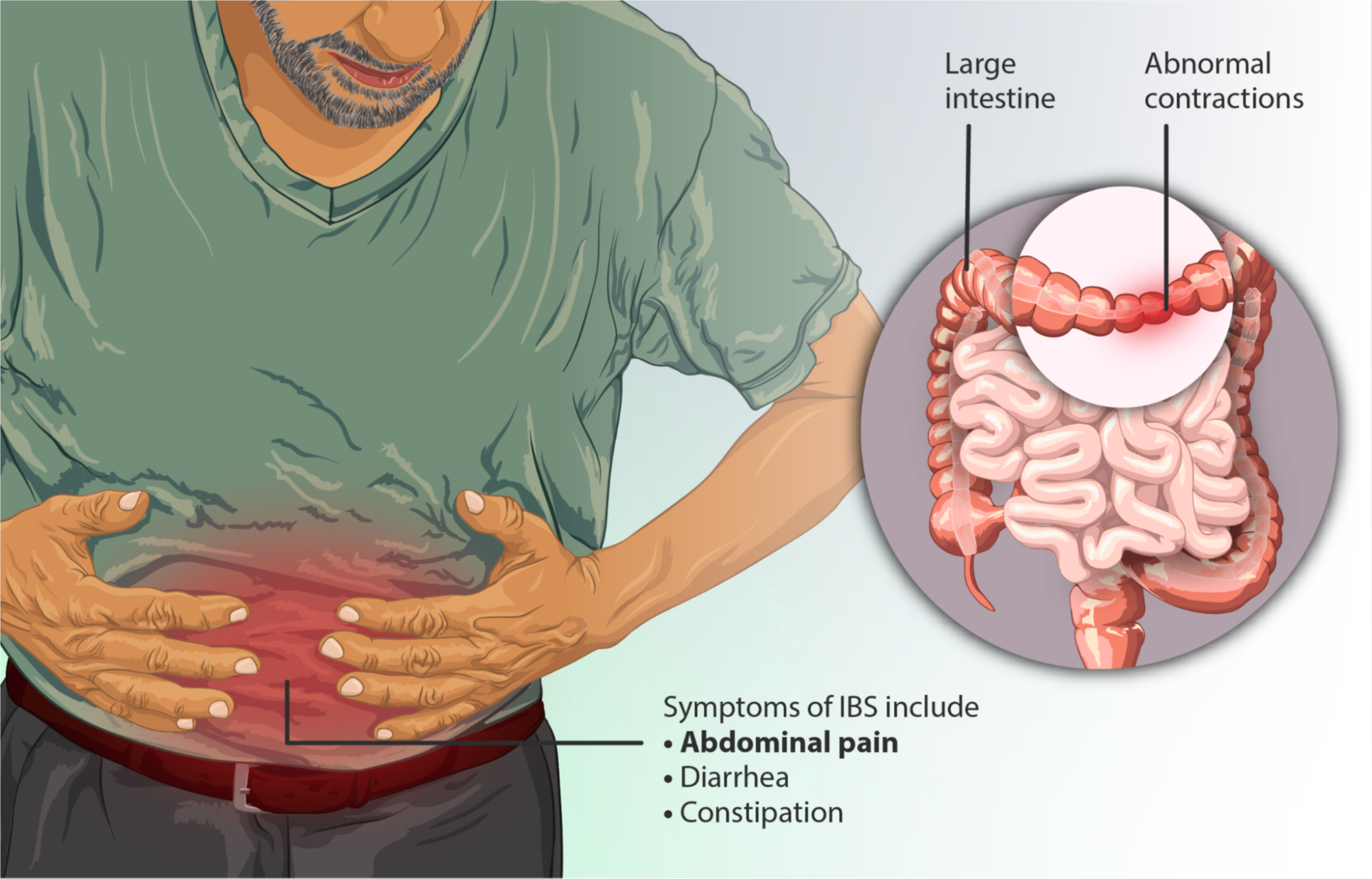
IBS is a gastrointestinal disorder characterized by a cluster of symptoms that can vary widely from person to person. At its core, IBS is a communication breakdown between the brain and the gut, leading to disruptions in the normal functioning of the digestive tract. This disconnect can manifest in a range of uncomfortable experiences, including abdominal pain, altered bowel habits, and a general sense of gut distress.
The Many Faces of IBS
IBS experience lies abdominal pain and discomfortOne of the hallmarks of IBS is the diverse array of symptoms that individuals may experience. While some people may grapple with persistent diarrhea, others may find themselves in a constant battle with stubborn constipation. In some cases, a frustrating pattern of alternating between the two can emerge, leaving patients feeling like their digestive system is in a state of perpetual upheaval.
Beyond the changes in bowel habits, IBS can also unleash a host of other disruptive symptoms. Bloating, gas, and abdominal discomfort are common companions, often exacerbated by certain trigger foods or stressful situations. In some cases, individuals may even experience mucus in their stool or a persistent feeling of incomplete evacuation after a bowel movement.
IBS Triggers
While some individuals may find that specific foods, such as dairy products or high-fiber items, consistently provoke their symptoms, others may struggle to pinpoint the culprits. Stress and anxiety also play a significant role in the IBS equation, as the brain-gut connection can amplify digestive distress during times of emotional turmoil.
Recognizing Symptoms & Reclaiming Gut Health
Navigating the diverse and often confusing landscape of IBS symptoms is the first critical step towards effective management. By becoming attuned to the unique patterns and triggers that shape your individual experience, you can begin to take control of your digestive well-being and embark on the path to relief.

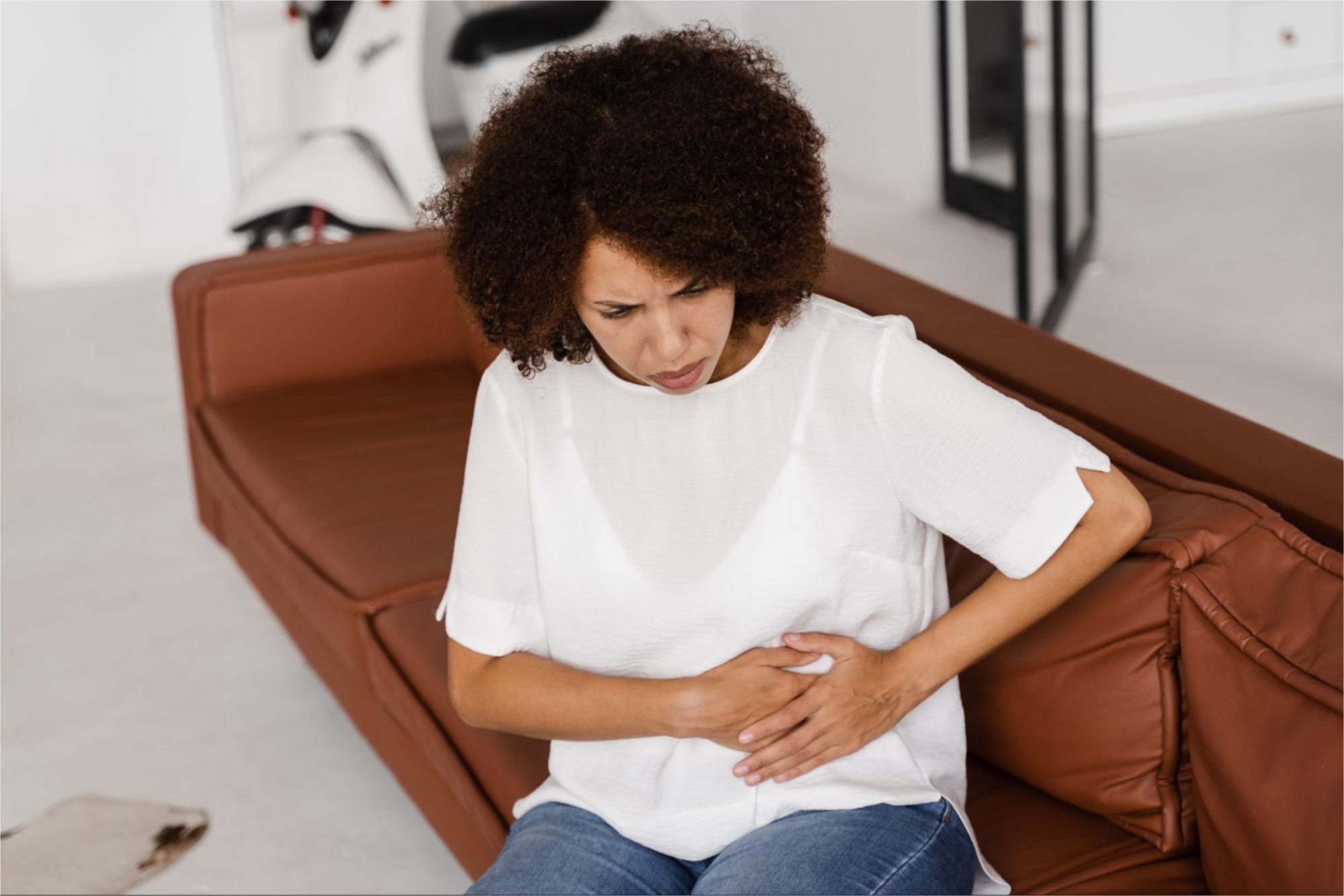
Abdominal Pain & Discomfort
At the heart of the IBS experience lies abdominal pain and discomfort. This disruptive symptom is often the primary driver that prompts individuals to seek medical attention. The pain may manifest as a dull ache, sharp cramps, or a general sense of unease in the gut, and it is often closely tied to changes in bowel habits.
One feature of IBS-related abdominal pain is its tendency to be relieved by bowel movements. Patients may find that the pain subsides after a successful trip to the restroom, only to resurface shortly after. This pattern can be frustrating and debilitating, leaving individuals feeling on edge and unable to engage in activities.
Altered Bowel Habits
Fluctuations in bowel habits are a hallmark of IBS, and the specific patterns can vary greatly from person to person. Some individuals may experience persistent diarrhea, while others grapple with stubborn constipation. In some cases, a frustrating cycle of alternating between the two can emerge, leaving patients feeling like their digestive system is in a state of constant upheaval.
The unpredictable nature of these bowel changes can be particularly challenging, as patients may never know what to expect from one day to the next. This lack of consistency can lead to feelings of anxiety and a sense of loss of control over one’s own body, further exacerbating the emotional toll of the condition.
Bloating, Gas, and Other Disruptive Symptoms
In addition to the primary symptoms of abdominal pain and altered bowel habits, IBS can also unleash a host of other disruptive experiences. Bloating and excessive gas are common companions, often triggered by certain foods or stressful situations. Patients may also report a persistent feeling of incomplete evacuation after a bowel movement, further adding to the sense of discomfort and frustration.

In some cases, individuals with IBS may even notice the presence of mucus in their stool, a symptom that can be both puzzling and concerning. While the appearance of mucus does not necessarily indicate a more serious underlying condition, it can be a source of anxiety and unease for those affected.
The Emotional Toll of IBS Symptoms
The unpredictable and often debilitating nature of IBS symptoms can take a significant toll on an individual’s emotional well-being. The constant worry about potential flare-ups, the frustration of managing a seemingly uncontrollable digestive system, and the social implications of the condition can all contribute to heightened levels of anxiety, depression, and stress.
It’s important to recognize that the emotional impact of IBS is not just a byproduct of the physical symptoms, but rather an integral part of the overall experience. Addressing the psychological aspects of the condition, in addition to the physical manifestations, is crucial for achieving a comprehensive approach to IBS management.
Irritable Bowel Syndrome Subtypes
While irritable bowel syndrome is often characterized as a single condition, it can actually be further categorized into distinct subtypes based on the predominant bowel habit patterns. Understanding these subtypes can be instrumental in tailoring treatment strategies and managing symptoms more effectively.

IBS with Constipation (IBS-C)
Individuals with IBS-C primarily experience persistent or recurring constipation, characterized by hard, lumpy stools and a sense of incomplete evacuation. This subtype can be particularly challenging, as the chronic nature of the constipation can lead to a host of additional discomforts, such as abdominal pain, bloating, and even nausea.
IBS with Diarrhea (IBS-D)
In contrast, IBS-D is marked by frequent, loose, and watery bowel movements. Patients with this subtype may find themselves constantly on the hunt for the nearest restroom, disrupting their daily routines and causing distress. The unpredictable nature of the diarrhea episodes can also lead to feelings of anxiety and a loss of control.
IBS with Mixed Bowel Habits (IBS-M)
Some individuals with IBS experience a frustrating cycle of alternating between constipation and diarrhea. This subtype, known as IBS-M, can be particularly challenging to manage, as the patient may never know what to expect from one day to the next. The constant fluctuations in bowel habits can be both physically and emotionally draining, requiring a tailored approach to treatment.
Understanding the nuances of these irritable bowel syndrome subtypes is crucial for healthcare providers and patients alike. By recognizing the specific patterns of bowel habits, individuals can work closely with their healthcare team to develop a personalized management plan that addresses their unique needs and symptoms.
Identifying Potential Triggers
Unraveling the mystery of IBS goes beyond simply recognizing the symptoms; it also involves identifying the potential triggers that can exacerbate or even induce these disruptive experiences. By becoming attuned to the factors that influence your digestive well-being, you can take proactive steps to manage your condition and minimize the impact on your daily life.

Dietary Culprits & Trigger Foods
One of the most common triggers for IBS symptoms is food we consume. Certain dietary components, such as fatty or spicy foods, caffeine, and alcohol, can wreak havoc on the balance of the digestive system. Additionally, foods high in fermentable carbohydrates, known as FODMAPs, can be problematic for individuals with IBS.
The Stress & Anxiety Brain-Gut Connection
The relationship between the brain and the gut plays a role in the IBS experience. Stress, anxiety, and other emotional factors can profoundly impact the functioning of the digestive system, leading to exacerbated symptoms or even triggering flare-ups.
Recognizing the influence of stress and anxiety on your IBS symptoms is crucial for developing a comprehensive management plan. Incorporating stress-reducing techniques, such as meditation, deep breathing exercises, or cognitive-behavioral therapy, can be instrumental in regaining control over your gut health.
Hormonal Fluctuations
For individuals assigned female at birth, the fluctuations in hormonal levels throughout the menstrual cycle can significantly impact the severity of irritable bowel syndrome symptoms. Many women report a noticeable worsening of their digestive distress during certain phases of their cycle, particularly around the time of their period.
Understanding the connection between hormonal changes and IBS can empower individuals to anticipate and prepare for potential flare-ups, allowing them to implement proactive strategies to mitigate the impact on their daily lives.
The Multifaceted Approach to IBS Management
Effective management of irritable bowel syndrome requires a multifaceted approach that addresses the physical, emotional, and lifestyle aspects of the condition. By working with healthcare providers and incorporating a range of evidence-based strategies, people with IBS can take control of their digestive well-being.

IBS Dietary Modifications
Dietary changes are often the first line of defense in managing IBS symptoms. By identifying and eliminating trigger foods, individuals can reduce the frequency and intensity of their digestive distress. The low-FODMAP diet, in particular, has gained widespread recognition for its effectiveness in alleviating IBS-related symptoms.
In addition to avoiding problematic foods, incorporating gut-friendly options, such as soluble fiber, probiotics, and anti-inflammatory ingredients, can help restore balance to the digestive system. Working closely with a registered dietitian can be instrumental in developing a nutrition plan that addresses your specific needs and preferences.
Medication & Supplementation
In some cases, healthcare providers may recommend medications or supplements to help manage the various symptoms associated with irritable bowel syndrome. It’s important to work closely with your healthcare provider to determine the appropriate type and dosage of any medication or supplement, as individual responses can vary.
Stress Management & Psychological Interventions
Recognizing the impact of stress and anxiety on IBS symptoms is a crucial step in developing a gut health management plan. Incorporating stress-reducing techniques, such as meditation, deep breathing exercises, or cognitive-behavioral therapy, can be instrumental in regaining control over your gut health.
By addressing the emotional and psychological aspects of IBS, individuals can not only find relief from their physical symptoms but also cultivate a greater sense of overall well-being. Healthcare providers who take a holistic approach, addressing both the physical and mental components of the condition, can be invaluable partners in the journey towards IBS management.
Lifestyle Choices for Gut Health
Engaging in regular physical activity, maintaining a consistent sleep routine, and avoiding triggers like caffeine or alcohol can all contribute to a more harmonious digestive system. By taking an active role in their own well-being and making intentional lifestyle choices, individuals with IBS can empower themselves to take control of their condition and minimize the disruption it causes in their daily lives.
Navigating the Gut Health Road Ahead
Recognizing symptoms of irritable bowel syndrome and understanding the triggers is just the first step in the journey towards gut health management. By working with healthcare providers, incorporating a multifaceted approach, and remaining persistent in the face of challenges, individuals with IBS can reclaim their digestive well-being and rediscover the joy of living without the constant burden of gut distress.
Remember, the road ahead may not be smooth, but with the right tools, support, and a willingness to explore various strategies, you can navigate the complexities of IBS and emerge stronger, more resilient, and in control of your own gut health. Your journey may have its ups and downs, but with the right mindset and a commitment to self-care, you can overcome the obstacles and find the relief you deserve.


0 Comments